Neurosurgery in Israel
The Top Ichilov Neurosurgery Department in Israel is headed by Professor Zvi Ram. Department neurosurgery in Israel uses all the advanced treatment methods known to the Israeli medicine. Twenty physicians, including five professors, work here. They are assisted by 47 certified nurses.
The department comprises 13 specialized clinics. These include clinics of pediatric brain and nervous system surgery, skull base surgery, stereotactic radiosurgery, brain catheterization, etc. Every year, the department experts perform about 2,500 surgical procedures, both open and minimally invasive.
Diseases
The department provides surgical treatment for all known diseases of the brain and spinal cord, peripheral nervous system and spine. Most patients come to the department to treat the following diseases:
| Astrocytoma | Brain aneurysm |
| Brain arteriovenous malformation | Brain tumor |
| Cerebellar tumors | Hemangioma |
| Glioblastoma | Glioma |
| Medulloblastoma | Meningioma |
| Neuroblastoma | Pituitary adenoma |
| Syringomyelia | Spinal stenosis |
| Spine injuries | Tunnel syndrome |
Leading Neurosurgeons In Israel
Patient treatment in Top Ichilov is provided by the leading specialists:

Professor Zvi Ram, Head of Neurosurgery Department at the Ichilov Medical Center. Has been performing brain surgery for about 40 years. Has mastered the awake craniotomy technique and the brain endoscopic stereotactic surgery performed without craniotomy, with special navigation systems. Operated and gave lectures in large university medical centers in Israel and the USA. Published about 200 scientific works.

Doctor Nevo Margalit, specialist in skull base surgery, has been working in the leading medical centers in Israel and the USA for about 20 years. Head of Neurosurgery Department at the Shaare Zedek Clinic. Performs endoscopic surgery for pituitary adenoma, trigeminal neuralgia, craniopharyngioma, and cerebrospinal fluid fistulae.

Professor Shlomi Constantini, specialist in pediatric surgery on the head. Director of Pediatric Neurosurgery Subdivision at the Ichilov Hospital. Performs open and endoscopic surgery for brain tumors. Provides surgical correction of congenital brain abnormalities as well as skull deformities in newborns. Has published over 270 scientific articles. Gives lectures at the Hebrew University of Jerusalem.

Professor Shimon Rochkind, Head of the Department of Peripheral Nerve Surgery at the Ichilov Medical Center. Performs microsurgical interventions on the brachial and lumbosacral plexus, including tumor cases. Provides patient rehabilitation after peripheral nerve and spinal cord injuries. Member of 23 international professional associations of physicians. Assistant professor of the Clinical Trial Department at the Tel Aviv University Faculty of Medicine.

Doctor Deborah Blumenthal, neuro-oncologist with over 30 years of professional experience, Head of Neuro-Oncology Clinic. Worked at the leading US clinics including MD Anderson Cancer Center. Author of 80 scientific works.

Doctor Ovadia Dror, spine surgeon, specialist in surgical treatment for scoliosis in children and adults. Head of the Pediatric Spine Surgery Clinic. Gives lectures on orthopedic surgery at Tel Aviv University.

Doctor Yigal Bronstein, spine surgeon, has been performing all types of spine surgery, including surgery for spinal disc herniation, for over 20 years. Worked at the leading clinics of Israel, Canada, and France.
Innovations: New Methods Of Diagnosis And Treatment In Top Ichilov
Laser Treatment for Epilepsy (LITT) Stops Seizures Completely
The laser interstitial thermal therapy technique is used for severe forms of epilepsy that do not respond to standard treatment. This is an alternative to craniotomy, open brain surgery that was historically performed in such cases. The minimally invasive, MRI-guided neurosurgical procedure is carried out through an incision in the skull. The diameter of the incision is less than 4 mm. Through this incision, the doctor ablates the problematic brain area where the seizures begin. The procedure does not affect healthy brain tissues.

This type of surgery significantly reduces the frequency of seizures or even makes them disappear completely in some patients. Clinical trials show that this method has fewer side effects compared to surgical treatment or radiation therapy.
Gliadel Wafers for Glioblastoma Treatment Double the Survival Rates
The capabilities of chemotherapy in brain tumor treatment are very limited. This is due to the blood-brain barrier, a natural filter preventing toxins from reaching the brain. The Gliadel wafers help overcome this barrier and deliver medication into the tumor area. The wafers contain carmustine, an antitumor drug. During surgery, the wafers are placed into the tumor bed. This is how medication reaches the brain directly to destroy any remaining tumor cells.
Clinical trials have shown that the wafers significantly reduce the risk of recurrence and virtually double the patient survival rates. According to clinical trial results, the use of Gliadel wafers significantly improves survival rates in glioblastoma patients.
The Optune Device Treats Brain Tumors and Improves Survival
The scientists developed a helmet to prevent cancer cells from growing. The electrodes on the device create special electric fields to block cancer cell division. The method is used for prevention of glioblastoma recurrence. Combined with other methods, the treatment substantially improves the overall survival rates. The clinical trials have shown an increase in average and 5-year survival rates in glioblastoma patients after electric field treatment.
Surgical Procedures At Neurosurgery Department Of The Top Ichilov Clinic
Craniotomy: Awake Brain Surgery
This is a surgical intervention performed under local anesthesia and sedation. To avoid disturbing important brain functions, doctors monitor the patient who is completely awake during surgery. Awake brain surgery is indicated for brain tumors. During the procedure, the patient remains conscious. Doctors ask them to complete easy, well-known tasks. This helps determine brain areas responsible for such major functions as movement, counting, speech, etc. Researchers presume that an awake craniotomy helps both remove as much tumor tissue as possible and preserve the patient’s cognitive functions.
Endoscopic Surgery without Opening up the Skull
The indications for endoscopic surgery include:
- Brain cysts;
- Pituitary adenoma and some other growths.
Surgery is performed without opening up the skull, or a craniotomy. Pituitary adenomas are treated using the transsphenoidal (transnasal) approach: endoscopic tools are inserted through the nostril. Cysts can be treated through small punctures in the skull.
Endovascular Surgery
Endovascular interventions occupy a special place in the Israeli neurosurgery. They are performed by vessel catheterization in an X-ray operating room. They are used for aneurysms and strokes. The procedures are carried out through a catheter inserted into the femoral artery. Patients stay in the hospital for 2-3 days. In 98% of cases, an endovascular procedure helps avoid open brain surgery.
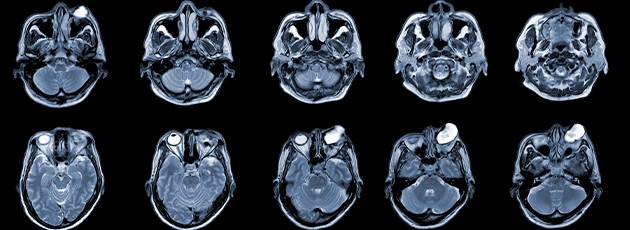
Radiosurgery Using the Gamma Knife System
This type of surgery is used for brain and spinal cord tumors as well as other head and neck growths. This is a single session of tumor irradiation using powerful gamma rays. Since the radiation is targeted, the surrounding healthy brain tissues are not affected. The specialist performs the procedure together with a radiation oncologist. After surgery planning using MRI, the experts proceed to targeted irradiation of the tumor. The procedure takes from 1 to 4 hours.
A Virtual Tour Of The Head And Nervous System Surgery Department

Before the procedure, the patient meets the neurosurgeon. The doctor explains the upcoming procedure and its expected results.

And this is our neurosurgical operating room. The advanced neuronavigation equipment helps perform brain surgery with pinpoint precision.

The awake craniotomy is a unique surgical procedure only performed in a few clinics of the world. These clinics comprise Top Ichilov. During surgery, the patient is not simply conscious; they solve math problems, draw or play musical instruments.
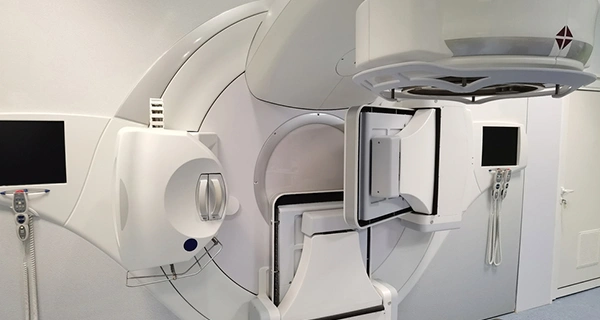
The radiosurgery system “Gamma Knife” destroys brain tumors as effectively as a surgeon’s scalpel.

Deep brain stimulation helps patients with Parkinson’s disease return to their fully functional lives.
Contact the Top Ichilov Medical Center
- Call the clinic right now: +972-37621629
- Or fill in the form below. Our doctor will contact you within 2 hours.

Publication Date:














